Why Use the Intrathecal Route for CNS Therapy?
The intrathecal route for CNS therapy plays a vital role in overcoming major challenges in drug delivery to the central nervous system. Traditional methods often fall short due to the highly selective blood-brain barrier. Scientists and medical professionals continuously seek effective means to address CNS disorders, where direct access to the brain can dramatically improve therapeutic outcomes. Its intrathecal route definition: refering to administering medication directly into the cerebrospinal fluid (CSF), typically via lumbar puncture or an implanted catheter, to deliver drugs around the brain and spinal cord. This approach bypasses barriers and enhances drug efficacy. This method not only allows for lower dosages but also significantly reduces systemic side effects, making it a preferable alternative for patients with neurological conditions. From neurological diseases to complex conditions like cancer, this delivery route showcases its utility. The growing prevalence of CNS disorders demands efficient treatments, and intrathecal administration stands out as a promising approach that addresses a critical need in drug development. Understanding its applications and benefits reveals its potential as a game-changer in therapeutic delivery.
CNS Drug Delivery Challenges and the Need for Intrathecal Routes
The Blood–Brain Barrier as a Major Drug Delivery Obstacle
The blood-brain barrier (BBB) is a formidable gatekeeper, safeguarding the brain from harmful substances circulating in the bloodstream. Composed of tightly packed endothelial cells, it permits selective permeability, allowing only essential nutrients and gases to cross its barrier. While this protective mechanism is crucial for maintaining the brain’s microenvironment, it poses significant challenges for drug delivery. Many therapeutic agents, especially large molecules and certain small molecules, fail to penetrate the BBB, rendering systemic treatments ineffective for CNS disorders. This limitation necessitates alternative delivery methods that can bypass this physiological barricade. Intrathecal administration presents a viable solution, enabling drugs to reach the CNS directly via the cerebrospinal fluid, circumventing the BBB and increasing the likelihood of therapeutic success. Addressing this obstacle is critical, as ineffective drug delivery can lead to inadequate treatment outcomes and the persistence of debilitating symptoms in patients.
Limitations of Systemic Administration for CNS Therapies
Systemic drug administration, despite being the conventional approach, often falls short in treating CNS disorders due to the blood-brain barrier’s selective nature. When drugs are administered systemically, they must first enter the bloodstream and then navigate through the barrier to reach the CNS. However, many drugs do not possess the physicochemical properties required for efficient BBB penetration, which results in suboptimal concentration levels reaching the target site. Additionally, systemic administration can lead to widespread distribution of the drug, increasing the risk of off-target effects and systemic toxicity. This can compromise patient safety and limit the use of potentially effective therapies. Moreover, higher dosages required to achieve therapeutic concentrations in the CNS may exacerbate side effects, further complicating treatment regimens. The inability to deliver drugs effectively and safely underscores the need for innovative delivery routes, such as the intrathecal method, which offers direct access to the CNS and minimizes systemic exposure.
How Intrathecal Administration Works in CNS Therapy
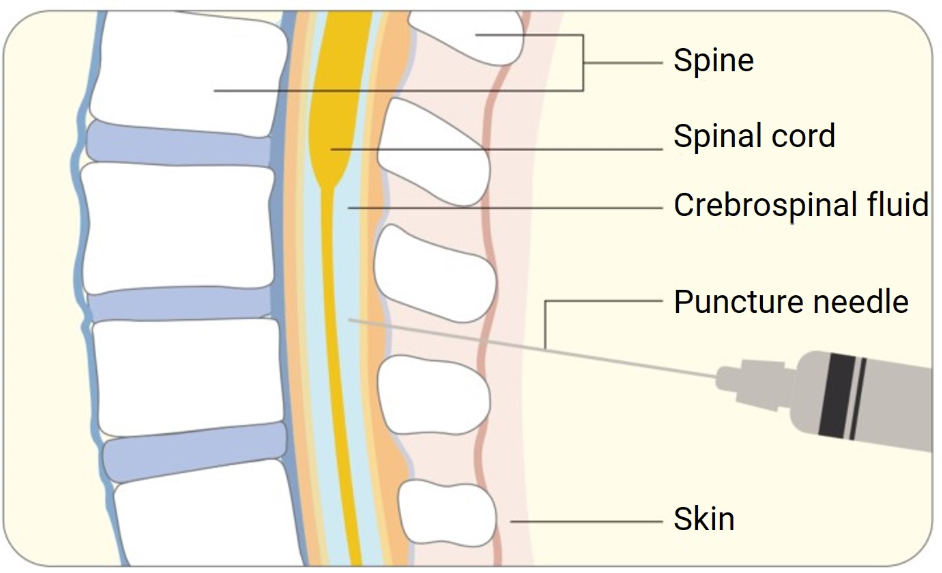
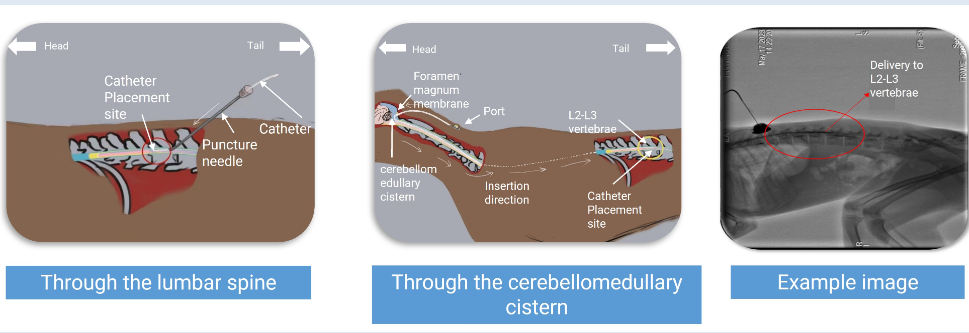
Mechanism of Intrathecal Drug Delivery via CSF
Intrathecal drug delivery is a targeted approach that involves the administration of therapeutic agents directly into the subarachnoid space, where cerebrospinal fluid (CSF) resides. This space, encompassing the brain and spinal cord, acts as the medium for drug distribution. Upon injection into the intrathecal space, the drug disperses through the CSF, allowing it to bypass the blood-brain barrier entirely. The close proximity to the CNS ensures that medications can exert their effects precisely where needed, enhancing therapeutic efficacy. This mechanism is particularly advantageous for delivering both macromolecules and small-molecule drugs that may not naturally traverse the BBB. Furthermore, this direct method of delivery facilitates rapid drug action, which is crucial for conditions requiring immediate intervention. Intrathecal delivery also allows for precise control over drug dosing, minimizing the volume required and consequently reducing potential side effects. Understanding this mechanism highlights why it is a preferred route for CNS-targeted therapies.
Pharmacokinetic Advantages of Intrathecal Dosing
The pharmacokinetics of intrathecal dosing offer significant advantages over traditional systemic administration. By delivering drugs directly into the CSF, intrathecal administration provides immediate access to the CNS, resulting in higher concentrations at the target site. This proximity ensures rapid onset of action and sustained therapeutic levels, which is crucial in managing acute CNS conditions. The localized nature of intrathecal dosing means that smaller doses can achieve desired effects, substantially reducing systemic exposure and toxicity. Moreover, this route of administration enables bypassing hepatic metabolism, which can alter drug efficacy when given systemically. Intrathecal dosing also allows for intermittent or continuous delivery, catering to diverse therapeutic needs and improving patient compliance. These pharmacokinetic benefits make it an attractive option for clinicians seeking to maximize treatment efficacy while minimizing adverse effects. By enabling precise and effective drug distribution within the CNS, intrathecal administration plays a pivotal role in advancing therapeutic options for CNS disorders.
Key Benefits of Using the Intrathecal Route in Drug Development
Enhanced CNS Exposure with Lower Systemic Toxicity
Intrathecal administration is designed to maximize drug delivery to the CNS while minimizing systemic exposure, providing significant therapeutic benefits. This route ensures that medications are concentrated directly in the cerebrospinal fluid, allowing targeted action on CNS tissues. The reduced requirement for higher systemic doses significantly lowers the risk of systemic toxicity, which is a major drawback of traditional systemic therapies. By decreasing the overall drug burden on the body, patients experience fewer side effects, thus improving the overall safety profile of treatments. This is particularly crucial for vulnerable populations, such as pediatric and geriatric patients, who may be more susceptible to adverse drug reactions. Ultimately, the enhanced CNS exposure coupled with reduced toxicity places intrathecal methodology at the forefront of innovative therapeutic strategies, offering a potent solution for effective treatment without compromising patient safety.
Applications in Rare, Neurodegenerative, and Oncology Diseases
Intrathecal administration holds promise for various challenging medical conditions, including rare disorders, neurodegenerative diseases, and CNS-related cancers. These conditions often entail significant hurdles due to the difficulty in achieving adequate CNS drug concentrations. For rare diseases, where tailored therapies are critical, intrathecal delivery offers a means of providing effective treatment directly to the site of pathology. In neurodegenerative disorders such as ALS and multiple sclerosis, this route facilitates sustained drug delivery, potentially slowing disease progression. Likewise, in oncology, where brain tumors present a formidable challenge due to the protective BBB, intrathecal administration allows chemotherapeutic agents to reach and impact tumor sites more effectively. The versatility of intrathecal delivery extends its applicability across a wide spectrum of CNS conditions, making it an essential tool in the therapeutic arsenal for conditions historically deemed hard to treat. Embracing this approach can lead to significant breakthroughs in CNS therapy development.
Conclusion
Intrathecal delivery represents a paradigm shift in CNS therapy, addressing the historic challenges posed by the blood-brain barrier. By facilitating direct access to the central nervous system, it provides a targeted, efficient, and safer means of drug administration. This method highlights unique pharmacokinetic advantages, allowing for rapid and sustained therapeutic effects while minimizing systemic exposure and reducing toxicity. With rising prevalence of CNS disorders, intrathecal administration’s role in drug development becomes increasingly relevant. It offers solutions for rare, neurodegenerative, and oncology diseases, indicating its versatility and potential for broader applications. By revolutionizing the way we approach CNS drug delivery, intrathecal methodologies promise enhanced treatment outcomes and improved quality of life for patients. As research advances, the continued exploration and optimization of this route may unlock further possibilities in therapeutic interventions within the complex landscape of CNS disorders.



